15 Jul The NHS has announced £20m for speeding up cancer diagnosis, but if they build it, will they come?
Having been parachuted into one of the most important jobs in the country at one of its most challenging times, Sajid Javid has expressed his shock at learning that the peak of the backlog is expected to reach 13 million people, up from an already staggering 5.3 million.
In this context, it’s welcome to see the NHS’ announcement earlier this week that the health service will be investing £20 million into speeding up cancer diagnosis across the country. The NHS Long Term Plan commitment to catch three quarters of cancers early – up from half at present – is becoming a pipe dream.
The new investment will include a range of innovative technologies for faster diagnosis of skin cancer, an increase in ‘lumps and bumps clinics’ where nurses will offer examinations and same-day ultrasounds, and a ‘cancer symptom hotline’ to allow people concerned with any symptoms to call up, speak with a nurse, and get a referral if needed.
But will the new initiatives have a significant impact on whether people come forward to get diagnosed early? Especially in the communities where low diagnosis is most prevalent and health inequalities more pronounced?
The underlying principle of the investment in quicker cancer diagnosis is that people want diagnosis to be less burdensome and more convenient.
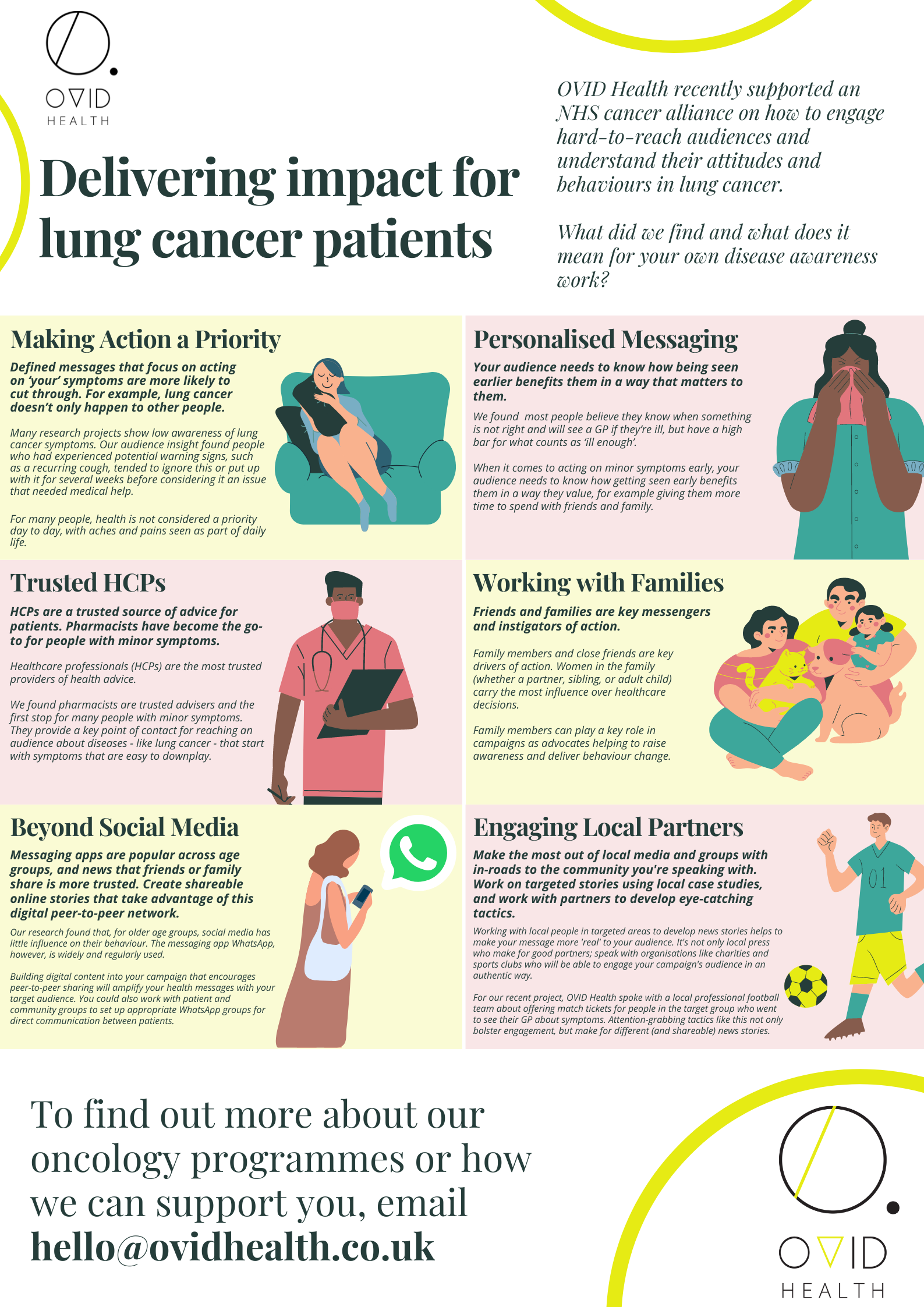
OVID Health has just completed a deep audience insight project on lung cancer symptom presentation for an NHS organisation in London. The client wanted to understand the drivers of late presentation during the pandemic in order to target behaviour change campaign in the most impactful way. In particular, the research focused on attitudes and behaviours in low-income, white British men and women between the ages of 55-79, living in the boroughs of Lewisham, Southwark and Lambeth.
Our research found that most people, if they felt there was something wrong with their health, they would seek help. The pandemic did not significantly impact their perception of the NHS or primary carer as “open for business”. The main barrier, it became clear, was that this demographic had a very high tolerance of being unwell, with few – even some experiencing chronic conditions – rarely considering themselves ‘ill enough’ to seek help.
Our unique research model gave deep insight that can help increase the success of symptom awareness and diagnosis campaigns. We were able to recommend several ways to engage people in their local area to not only raise awareness about warning symptoms, but to show them why getting this checked mattered. We’ve captured the key takeaways in an infographic which you can see below, as well as download here.
If you are looking to carry out audience insight research in health or build practical recommendations for cancer campaigns, or would like to discuss our insights further, get in touch with us at [email protected].